I attended a “State of the Industry” presentation by Daniel Kuzmanovich from The Advisory Board yesterday. Daniel did an outstanding job presenting a lot of powerful research about the healthcare industry. If you haven’t seen this presentation or know about The Advisory Board, I encourage you to sign up. I grabbed a few slides from Daniel’s presentation to comment from the perspective of an organization that guides hundreds of patients to high value surgeons each month and will comment on a few of the more salient points on this platform.
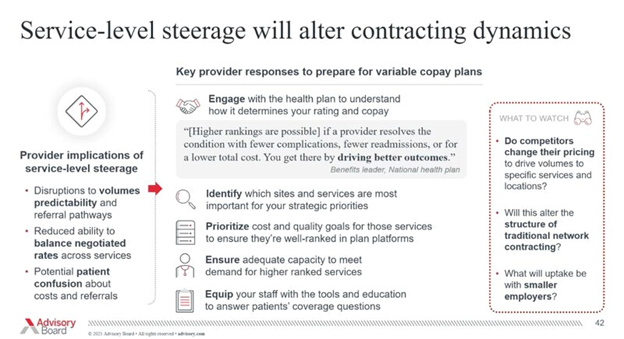
The slide is from the perspective of a health system or ASC. Looking at this from an Employer’s standpoint, it’s clear that health systems and most ASCs have no idea who is controlling their steerage. Spoiler alert: It’s NOT the network. If your ASC “consultant” ever says, “just sign up with UHC and you won’t have to worry about referrals” (and I know an ASC who was told this), fire the consultant and move on.
If a health system or surgical practice is going to make the effort to create value based bundled pricing and is capturing quality data, network contracting is an important step, but it won’t increase market share. The value of the bundle and the practice MUST be communicated to the insurance broker and employer HR communities so they can build steerage into benefit plan designs.
Alithias has helped surgeons, ASCs, brokers and networks follow this successful strategy to get patients to the highest value doctors. The result is proven cost savings and better outcomes. Please contact me if you’d like help creating bundles, building an incentive based benefit plan design, or if you need an advocacy company to guide employees to the best healthcare values.
In short:
1) Service Level steerage WILL alter contracting dynamics
2) There WILL be patient confusion about cost and value
3) If the doctors do not define their quality, someone else will do it for them
4) Competitors will eventually change their pricing to market rates once bundled rates are established
5) Employers will refer patients based on quality and value ONLY if they have an incentive based benefit plan design.
A final note: This does not have to be a race to the bottom for provider organizations. There are ways to reduce contract risk and get more patients. If you want to know how, DM me
Activate to view larger image,